Laser Peripheral Iridotomy Procedure
Since their development nearly 50 years ago, lasers have revolutionized many fields, particularly medicine. Lasers allow us to easily and safely perform procedures which were once much more invasive, or not possible at all.
A laser is basically a very focused beam of light energy. The color of light emitted by a laser is determined by the type of material used to produce it. This material can be a gas, a liquid, a solid, or a semiconductor such as a diode. When the material inside the laser tube is energized, it produces light of a very specific wavelength, or color. In ophthalmology, lasers range in wavelength from infrared to ultraviolet. The wavelength determines how the laser will affect different cells and tissues within the body. The ability to control the exact amount of energy delivered by the laser makes it the perfect tool to perform precise, delicate surgery within the eye.
Anatomically Narrow Angles
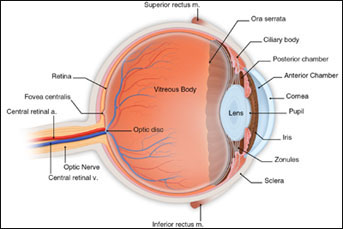
The anterior chamber angle is formed where the peripheral cornea and iris meet. At the apex of this angle lies the trabecular meshwork, the sieve-like entrance to the ocular drainage system. Aqueous humor, the fluid which fills the front of the eye, is constantly being created. Anatomy of the eye This fluid must therefore flow out through the trabecular meshwork in order to maintain the proper pressure within the eye. If the drainage system becomes blocked, aqueous humor cannot escape and pressure will build, potentially damaging ocular structures.
In most cases, narrow angles are a genetically determined condition. Affected individuals are usually hyperopic (farsighted) with shorter than average eyes. Women are affected more often than men, and the condition often worsens with age. Individuals of Asian or Eskimo ancestry appear to be at greater risk for narrow angles.
Plateau iris, another abnormal condition associated with angle narrowing, occurs due to abnormal anatomy in the ciliary body, causing the iris to be pushed too far forward. This condition is less common than that previously described, and will not be detailed here.
Other conditions can occasionally be associated with narrow angles. For example, a very thick, mature cataract can compromise the angle, causing high pressure. This is resolved by cataract surgery.
Two significant problems may result from narrow angles:
Chronic IOP elevation: Increased resistance to aqueous humor outflow can lead to a chronic elevation in intraocular pressure, known as chronic angle closure glaucoma. This condition often behaves like the more typical open angle glaucoma, with moderately elevated pressures, no pain, and slow but progressive loss of visual field.
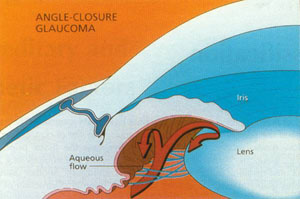
Nausea and vomiting are common, as are colored halos around lights. If not treated urgently, acute angle closure can cause permanent loss of vision. The condition is often precipitated by partial dilation of the pupil. This may occur upon entering a lighted space after being in prolonged darkness, with excercise or excitement, or even with pharmacologic dilation during an eye exam. Individuals with a history of narrow angles should seek medical attention if the above symptoms occur.
Laser Peripheral Iridotomy (LPI)
As noted previously, aqueous humor is produced by the ciliary body in the posterior chamber of the eye, the space behind the colored iris. This fluid normally passes through the pupil and into the anterior chamber, the space in front of the iris. Aqueous then drains into the trabecular meshwork and out of the eye. However, in narrow angles, fluid cannot move through the pupil normally, due to excessive contact between the iris and lens. Fluid builds up behind the iris, pushing it forward, further narrowing the angle and leading to acute closure in predisposed individuals. This situation is known as pupillary block (see diagram above), and is the most common cause of acute angle closure.
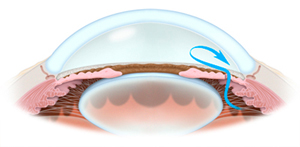
Flow of aqueous humor through a peripheral iridotomy The iridotomy is therefore completely within the eye- it is not a hole in the eyeball. This opening allows the aqueous humor to pass freely through the iris and into the trabecular meshwork. An iridotomy acts as a low-resistance”bypass,” giving aqueous a clear pathway into the drainage system. In most cases the iris will actually move slightly backwards after iridotomy, as there is less pressure built up behind it. This deepens the anterior chamber, opening the angle wider, further facilitating the outflow of aqueous humor from the eye. Laser iridotomy is therefore the initial treatment of choice for patients with chronic angle closure. It is also the best means of prophylactically reducing the risk of acute angle closure in patients predisposed to the condition.
If your physician determines that your angles are significantly narrow, putting you at risk for acute angle closure, peripheral iridotomy many be recommended.
The Laser Iridotomy Procedure
Laser iridtomy is a brief, in-office procedure. Many patients are able to drive to and from their appointment alone, though blurry vision may occur after the procedure and a driver may be desired. The actual procedure is described below:
- Prior to the procedure, pilocarpine drops will be placed in the eye to be treated. This medication constricts the pupil, tightening the iris and making the iridotomy easier to perform.
- You are seated at a slit-lamp microscope, similar to the type used to examine your eyes during a regular appointment.
- Anesthetic eye drops are given.
- A special lens is placed on the treated eye. This lens helps to keep the eye open and still, as well as to focus the laser. Your eye is numb; you will not feel any discomfort from this.
- As the procedure begins, you will be asked to look slightly down, or at a provided fixation target.
- During the procedure, which lasts justs a few minutes, you will see a flashing light and will feel a very brief pinch in the eye as the laser pulses. This can be startling, however the discomfort is usually minor. Rarely, more discomfort may be felt and the procedure can be adjusted to limit this.
- The number of laser pulses required to penetrate the iris and create an appropriately sized opening depends upon the thickness of the iris. Patients with dark colored irides often require more laser pulses then those with light colored irides, and may therefore feel a bit more discomfort.
- Once the treatment is complete, the lens is removed and the eye is rinsed with saline. Eye drops are given for comfort.
- You may be asked to remain in the office for up to one hour to check the intraocular pressure following the procedure.
- You will be given anti-inflammatory eye drops to be used for a few days, as directed by your surgeon.
- During the few days following the treatment you may experience slight blurred vision, discomfort, light sensitivity, and redness in the treated eye. These symptoms should all be very mild and should not limit your activities in any way. There are no restrictions following the procedure.
- In general, any pre-treatment glaucoma medications will be continued until the long-term effect of the laser procedure is known. A follow up appointment will usually be made within 1 to 2 weeks of the treatment.
Risks of Laser Iridotomy
All laser procedures have some risk. Risks of iridotomy include:
- Bleeding: A small amount of bleeding from the iris is quite common and usually stops in less than a minute with brief pressure against the eye. In extremely rare cases, prolonged bleeding may occur, requiring further medical or surgical treatment
- Elevated intraocular pressure: Usually transient and brief, a rise in IOP may require additional medication. Rarely, IOP may remain elevated for a longer period. This is more likely to occur in patients being treated for chronic angle closure. In such cases, continued use of medications, additional laser surgery, or filtering surgery might be necessary.
- Intraocular inflammation and formation of adhesions between the iris and lens. Anti-inflammatory drops are used post-treatment to avoid this.
- Corneal abrasions can occur during removal of the iridotomy lens. These are painful but heal quickly and are generally benign.
- Retinal problems, including macular edema (swelling) or retinal tears/detachments. These are rare but may require medical or surgical treatment by a retinal specialist.
- Cataract formation: Some studies suggest that cataracts, which develop normally with age, may occur a bit earlier in patients who have undergone iridotomy. Very rarely, rupture of the lens capsule may occur, leading to acute cataract formation.
- Halos, glare, double vision. Light passing through the iridotomy may occasionally cause glare or frank double images. The greatest risk of these symptoms occurs when the iridotomy is placed near the upper eyelid margin. Care is taken to place the iridotomy in a position that is well-covered by the eyelid, avoiding these problems.
- Closure of the iridotomy: Iridotomies performed with the YAG laser remain open 90 to 95 percent of the time. Infrequently, due to inflammation, they may close and require repeated laser treatment.
- Failure to complete the iridotomy: In patients with very thick irides, an iridotomy might not be completed during a single visit. In such cases, a second treatment is performed on another day to finish the procedure.
The above list of complications is provided for informational purposes. Iridotomy is a very commonly performed procedure which is quite safe. Serious complications are very rare. The risk of any complication is generally outweighed by the risks of not performing the iridotomy. Acute angle closure can be devastating, causing permanent damage to the eye, and is preventable in more than 95% of cases by prophylactic iridotomy. Please discuss all concerns with your surgeon.
If you have any questions about this or any other procedure, please feel free to contact us for more information.
