“EXCELLENT SURGEONS THAT ARE CARING PEOPLE, TOO!”
The #1 Glaucoma Management in Tucson and Nearby Areas
Glaucoma is a group of eye disorders that can lead to progressive loss of vision, often without any symptoms. Visual loss results from damage to the optic nerve, which transmits signals from the eye to the brain, much like an electrical cable. Once nerve fibers are damaged by glaucoma, the information they supply can no longer reach the brain. Peripheral vision is usually lost first.
Because central vision is preserved until late in the disease and pain is usually absent, most people with glaucoma don’t realize that anything is wrong.
To ensure that you have the greatest chance of success, trust a qualified team to care for your eye health.
-
Customized LASIK, PRK, and ICL Surgery
If you’re in the Tucson and Oro Valley area, you will find an experienced eye surgeon at Fishkind, Bakewell, Maltzman & Hunter Eye Care and Surgery Center.
5-Star Rated Glaucoma Management in Tucson.
Hear What Our Customers Say
A general overview
Diagnosing For Glaucoma Management in Tucson
Unfortunately, the diagnosis is glaucoma is not always straightforward, even after all testing is performed. There is significant variation in the appearance of normal optic nerves, with many healthy nerves looking a bit suspicious for glaucoma. Because glaucoma is usually a very slowly progressive disease, it is not uncommon for patients to be watched carefully without treatment while the diagnosis of glaucoma is considered. These ‘glaucoma suspects’ may be followed for many years before a final diagnosis is made and treatment is initiated. If suspicion is relatively low, ‘watchful waiting’ avoids the potential risks and side effects of treatment.
Your physician will perform a complete medical history and eye examination in order to determine your risk factors and search for signs of disease. The entire eye will be carefully evaluated, with special attention paid to the optic nerve, the structure damaged by glaucoma. The optic nerve is viewed through your dilated pupil using a special lens and an ophthalmic microscope. Gonioscopy may also be performed, in which a special mirrored lens in placed on your eye in order to directly examine the drainage angle and trabecular meshwork. The thickness of your cornea may also be measured, as an abnormally thick or thin cornea can affect the accuracy of intraocular pressure measurement. After your exam, if glaucoma is suspected, additional tests may be recommended.
Stereoscopic optic nerve photographs are taken with a specialized camera system, providing true, three-dimensional images of the optic nerves. These photos can be repeated over time and examined for signs of progressive nerve damage. In order to obtain clear photos, pupillary dilation is required. This examination usually takes about 45 minutes, including the time required for dilation.
Visual field testing is conducted to evaluate the function of the optic nerve. As glaucoma damage progresses vision is lost, typically beginning in the periphery and moving toward the center. Computerized visual field devices flash a series of lights in your peripheral vision in order to map out any areas of visual loss. Again, by repeating this test over a period of time, stability or progression of the disease can be ascertained and treatment adjusted as necessary. Completion of this test can take anywhere between 20 and 45 minutes, depending upon the exact type of examination your doctor orders. Your eyes will not be dilated for a visual field.
Ocular Coherence Tomography, or OCT, uses a laser to create a three-dimensional image of the optic nerve and surrounding retina, which is then analyzed by a computer. This allows your physician to better evaluate the structure of the fibers of the optic nerve, which are altered by glaucoma. Changes in the structure of the optic nerve occur early in glaucoma, often preceding any visual changes, and identification of these changes may be the best way to diagnose the disease. By repeating this exam over time, the success of glaucoma treatment can be monitored. The performance of this test usually does not require dilation and takes about 15 to 20 minutes.


What Are the Risk Factors of Glaucoma?
A number of risk factors for the development of glaucoma have been identified:
-
High intraocular pressure: IOP above 21 is considered high, and with increasing pressure comes an increased risk of glaucoma. However, not all high pressure will lead to glaucoma.
-
Race: African Americans are five to six times more likely than Caucasians to be affected by the disease, which tends to be more severe and progress more quickly in this population. Latinos are also at greater risk than Caucasians. The reasons for these racial differences are not well understood but are most likely genetic.
-
Family History: History of glaucoma, particularly in a first-degree relative, i.e. parent or sibling, increases one’s risk. The genetics of glaucoma, however, are usually not simple, and there is no way to predict which family members will be affected.
-
Age: Glaucoma is uncommon under 40, but risk increases with each decade of life.
-
Blood Pressure: High blood pressure has been associated with increased intraocular pressure in some studies, but it remains unclear exactly how significant this association is clinically.
Low blood pressure may be a risk factor for glaucoma progression, particularly in patients with low tension glaucoma, a form of open-angle glaucoma in which the pressure is in the normal range, often quite low.
-
Sleep-associated breathing disorders: Disorders such as sleep apnea, may be a risk factor, particularly for low tension glaucoma, again due to abnormal blood flow to the optic nerves.
Other possible risk factors include diabetes and myopia (nearsightedness), however studies have provided inconsistent results as to the degree of association with these factors.
What Types of Treatments are Available in Glaucoma Management?
Treatment for glaucoma is individualized for each patient’s specific condition. There are three basic options available, all of which serve to lower the intraocular pressure. After medication, Laser Surgery and Micro-Invasive Glaucoma Surgery, or MIGS procedure, are options to treat your glaucoma.
-
Medications
Medications lower pressure by either decreasing the production of fluid within the eye or by opening the drainage system to allow more fluid out. There are numerous classes of medications available, each with its own set of side effects. Your doctor will suggest medications for you based upon their safety and efficacy, taking your general health and use of other medications into account.
-
Micro-bypass stents
This is a Micro-Invasive Glaucoma Surgery, or MIGS procedure, attempting to reestablish good flow through the eye’s normal drainage system. Currently, there are two types of stents available for implantation in the United States, the Glaukos® iStent®, which is now in its third generation is known as the iStent Inject®, and the Ivantis® Hydrus® microstent.
Initially approved by the FDA in 2012 and 2018, respectively, these stents are inserted through the trabecular meshwork and into Schlemm’s canal in order to drain aqueous humor more effectively. On average, however, these stents lead to pressure reduction of one to two millimeters of mercury beyond that produced by cataract surgery alone and decrease the need for medications by one to two drugs. There is minimal additional risk to the implantation of these stents, and no impact on the normal healing period for cataract surgery. In general, blood thinners do not need to be stopped. The decision regarding which stent to implant is best made based upon the anatomy of the individual eye, conditions found at the time of surgery, and the surgeon’s familiarity with each device.
-
Ab-Interno Canaloplasty (AbIC)
This MIGS procedure dilates and cleans out Schlemm’s canal. A tiny catheter, or hollow tube, is inserted into the canal through the trabecular meshwork and passed 360 degrees around the entire eye, breaking adhesions and scar tissue that have formed over time.
As the catheter is withdrawn, a thick liquid is injected into the canal, further dilating it and forcing out debris. This procedure is effective and reimbursed by insurances either combined with cataract surgery or when performed by itself. Several reasonably sized studies have shown pressure reductions of as much as 30%, or four to six millimeters of mercury, though actual reduction may be more or less than this. Complication rates are relatively low and generally mild, though bleeding is more likely than with stent implantation and therefore discontinuation of blood thinners is recommended for this procedure. Recovery to clear vision may be slightly delayed by a few days due to bleeding.
-
Trans-scleral Stents
This procedure bridges the gap between MIGS procedures and traditional filtering surgery. Like filtering surgeries, aqueous humor is diverted from inside to outside the eye via a bypass through the sclera, forming what is known as a “filtering bleb.” However, much less cutting and manipulation of tissues is required when implanting these devices, with considerably shorter operative and recovery times.
Some of the risks of traditional filtering surgery are reduced, though certainly not eliminated. Therefore, unlike other MIGS procedures that can be performed by nearly any eye surgeon trained appropriately, trans-scleral stents are generally implanted by surgeons experienced with glaucoma filtering surgeries and their post-operative management. There is only one such device approved for use in the US by the FDA: the XEN45 glaucoma implant. Another such implant, known as the PreserFlo shunt, is expected to be approved in 2021.
-
Laser Trabeculoplasty
This laser treatment relieves intraocular pressure by stimulating the internal drainage system allowing adequate outflow of fluid from the eye. There are two types of laser trabeculoplasty procedures: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT)
The original procedure, described in 1979, was performed using an argon laser, though currently a solid-state diode laser is often employed. These lasers produce light in the visible spectrum with a blue-green color. This type of treatment is often called “argon laser trabeculoplasty,” or ALT. ALT is a time-tested procedure which has been performed for over 40 years. The greatest drawback to ALT is that it can only be performed two to three times on an eye, as further treatments can actually cause injury. A newer version of the procedure, known as “selective laser trabeculoplasty,” or SLT, achieves the same goal using a frequency-doubled neodymium:YAG laser, also producing light in the blue-green spectrum. Because the amount of energy delivered by this laser is less than that in ALT, the procedure can theoretically be repeated as many times as desired without risk of injury to the eye. Multiply repeated treatments performed years apart are often successful. Presently, we perform primarily the SLT procedure, based upon its better safety profile and ability to be repeated multiple times, as needed. Trabeculoplasty will not cure glaucoma. Damage to the optic nerve cannot be reversed. The goal of trabeculoplasty, as with all treatments for glaucoma, is to lower intraocular pressure and prevent the further loss of vision. In some cases, glaucoma medications may be eliminated, however many patients will need to continue all pre-treatment eye drops to maintain adequately low IOP. Trabeculoplasty is not 100% effective at lowering intraocular pressure. Results often vary depending upon the type of glaucoma, number and type of eye drops being taken, and other conditions affecting the eye. Your surgeon will discuss your specific situation and will provide appropriate guidance.
-
Laser Peripheral Iridotomy (LPI)
This laser treatment makes a small opening in the peripheral iris (the colored part of the eye). This changes the fluid dynamics in the eye and “opens” the angle. If a patient already has acute angle closure glaucoma, the small opening that is made in the peripheral iris allows fluid to drain more normally and also lowers the eye pressure.
The Iridotomy acts as a low-resistance”bypass,” giving aqueous a clear pathway into the drainage system. In most cases the iris will actually move slightly backwards after iridotomy, as there is less pressure built up behind it. This deepens the anterior chamber, opening the angle wider, further facilitating the outflow of aqueous humor from the eye. Laser iridotomy is therefore the initial treatment of choice for patients with chronic angle closure. It is also the best means of prophylactically reducing the risk of acute angle closure in patients predisposed to the condition.
See Now – Pay Later! Finance Your LASIK Procedure with CareCredit!

Why Our Facility Is a Great Glaucoma Management Center for You
We know that you have a choice of teams and locations for your care. Our team of experts look forward to providing the highest quality care. Our experienced team, high-tech equipment, and personalized care provide you with the best outcomes for your vision.
FAQ
Glaucoma Questions & Answers
Scientist are not entirely sure what exactly causes Glaucoma. Ultimately the passages that allow the fluid within your eye to drain are blocked. Because of that, fluid builds up in your eye and causes an increase in pressure on the optic nerve. The optic nerve and blood vessels are damaged by the increased pressure, which can result in vision loss.
Glaucoma can cause blindness, but it can be prevented. If it is diagnosed at an early stage, the damage can be controlled. If treatment is delayed, you are likely to lose peripheral vision first and then the central vision, which may result in complete blindness.
Glaucoma often does not have obvious symptoms. Additionally, symptoms may not show until it is already too late.
If you have open-angle Glaucoma, the initial symptom might be vision loss – which is a sign of damaged optic nerve.
If you have closed-angle closure Glaucoma, initial symptom may be blurry vision. You might also see rings or halos around lights. You may experience pain or strain in your eye and they may also get red.
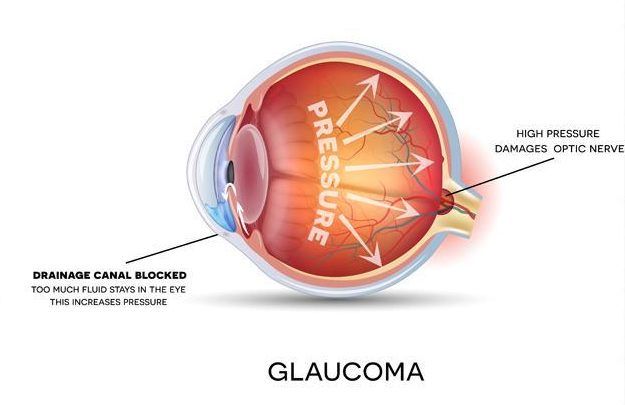
Glaucoma is usually broken down into two major categories: open-angle glaucoma and closed-angle glaucoma.
In open-angle glaucoma, the drainage canals are correctly formed but are slow clogging, resulting in increased eye pressure.
In closed-angle glaucoma, the entrance to the trabecular meshwork becomes blocked by the iris, which assumes an abnormally forward position. This causes the drainage canal to become narrow and eventually close. Unlike symptom-free open-angle glaucoma, this condition, sometimes called “narrow-angle glaucoma,” often presents suddenly, with pain, red eye, tearing, and colored haloes around lights. Vision can be lost quickly, and urgent treatment is required.
Meet Our Glaucoma Specialists