Glaucoma : Angle Closure and Narrow Angles
Narrow Angles and Angle Closure Glaucoma
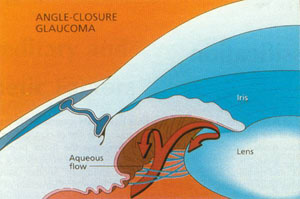 Closed angle glaucoma is relatively uncommon compared with the typical open angle form. In open angle glaucoma the entrance into the trabecular meshwork is unobstructed, though an abnormality deep within the meshwork leads to elevated intraocular pressure. In closed angle glaucoma, the entrance to the trabecular meshwork becomes blocked by the iris, glaucoma4 which assumes an abnormally forward position. Aqueous humor cannot gain access to the trabecular meshwork and drainage canals, causing the intraocular pressure to increase.
Closed angle glaucoma is relatively uncommon compared with the typical open angle form. In open angle glaucoma the entrance into the trabecular meshwork is unobstructed, though an abnormality deep within the meshwork leads to elevated intraocular pressure. In closed angle glaucoma, the entrance to the trabecular meshwork becomes blocked by the iris, glaucoma4 which assumes an abnormally forward position. Aqueous humor cannot gain access to the trabecular meshwork and drainage canals, causing the intraocular pressure to increase.
People with closed angle glaucoma often have a shorter than average eye in which all the internal structures, including the cornea and the iris, are closer together than normal. Many of these individuals are hyperopic, or farsighted. Others have a condition called plateau iris, in which the iris is attached too far forward in the eye. With age, the eye’s lens thickens, pushing the iris further forward and narrowing the angle. Eventually the angle can become completely blocked by the peripheral iris, preventing the flow of aqueous humor from the eye. This leads to elevated intraocular pressure and optic nerve damage.
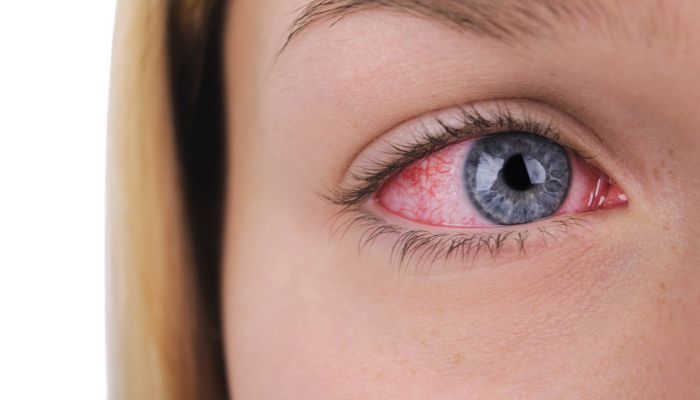
Unlike symptom-free open angle glaucoma, this condition, sometimes called “narrow angle glaucoma” or “acute angle closure,” often presents suddenly, with pain, red eye, tearing, and colored haloes around lights. Vision can be lost quickly, and urgent treatment is required. In other cases the closure of the angle is slow and progressive, leading to a condition more like open angle glaucoma, with slow damage and no symptoms.
Risk Factors for Angle Closure Glaucoma
- Hyperopia. Being farsighted is a major risk factor for narrow angles and angle closure. Hyperopic eyes tend to be short, causing crowding of the angle structures and narrowing the angle.
- Race. Many Asians and Eskimos have shallow anterior chambers, predisposing them to angle closure.
- Age. As we age, the lens becomes thicker and larger, increasing the risk of angle closure in predisposed individuals.
- Sex. Women are 2-3 times more likely than men to suffer angle closure.
Treating Narrow Angles/Angle Closure Glaucoma
Narrow angles and angle closure glaucoma, while often treated with some of the same medications and surgical procedures as open angle glaucoma, have one notable difference. In these conditions, the problem of a narrow angle caused by the iris and cornea being too close together is often exacerbated by a situation known as pupillary block.
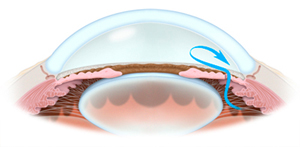
Flow of aqueous humor through a peripheral iridotomy Due to resistance of flow at the pupil , there is actually a slightly higher pressure behind the iris than in front, and this tends to bow the iris forward, contributing to the already narrow angle, and further blocking outflow of fluid from the eye. This papillary block is commonly the cause of acute angle closure in predisposed individuals. Treatment is aimed at alleviating this condition.
A laser is used to create a small opening (or openings) in the periphery of the iris. Known as laser peripheral iridotomy, this procedure creates a lower resistance pathway for aqueous to pass from behind to in front of the iris, preventing papillary block and significantly reducing or eliminating the risk of acute closure of the angle. Iridotomy is effective and safe, with little risk of significant complication. The same procedure is required emergently to treat an actual attack of angle closure, however is much more difficult to perform and may be too late to prevent permanent damage to the eye. Therefore, if your physician finds narrow angles, laser iridotomy may be recommended on a prophylactic basis.