Glaucoma: Filtering Surgery – Glaucoma Drainage Devices
When medications or laser procedures fail to adequately control intraocular pressure (IOP), or if side effects prevent the continued use of medications, surgery becomes necessary to achieve the desired level of IOP. Surgery for glaucoma lowers IOP by either increasing the flow of fluid out of the eye or by decreasing the production of intraocular fluid.
It must be remembered that the optic nerve damage and subsequent loss of vision caused by glaucoma cannot be reversed. Thus, the point of surgery is not to improve vision, but rather to prevent further vision loss. Currently there is no glaucoma treatment that can restore vision already lost to the disease. For this reason, early diagnosis and treatment are vital. We recommend reading the section about glaucoma before continuing here.
This article describes glaucoma drainage devices, a commonly performed surgical procedure used to treat many forms of glaucoma.
Introduction
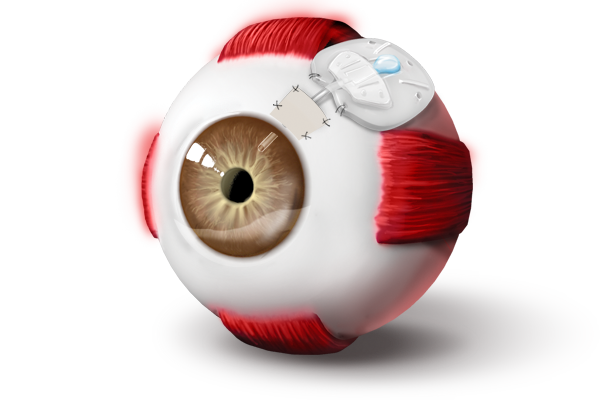
Known as a “glaucoma drainage device,” “tube shunt,” “glaucoma valve,” or “Seton,” this procedure is often performed after other forms of glaucoma filtering surgery, most commonly trabeculectomy, have failed to adequately control intraocular pressure (IOP). Increasingly, however, it is being performed as an initial filtering procedure, and is usually the procedure of choice in cases considered high risk for trabeculectomy failure, such as neovascular or inflammatory glaucoma. A drainage device consists of a small tube which is inserted into the eye, usually into the anterior chamber near the edge of the cornea, and a plastic plate which is placed outside the eye beneath the conjunctiva, the clear membrane which covers the eye. The plate serves a bit like a reservoir, creating a space for aqueous humor to collect, much like the bleb in trabeculectomy.
For simplicity, think of glaucoma as being caused by a clogged drain. Aqueous humor is constantly being created but cannot escape quickly enough, building up pressure and damaging the optic nerve. The drainage device gives the fluid a low resistance means of escape, leading to lower, better controlled pressure. The fluid which leaves the eye via the tube drains into the space around the plate, beneath the conjunctiva, before being reabsorbed into the bloodstream.
A number of drainage devices are available from various manufacturers, varying in overall shape and size. The most significant difference between devices is the presence or absence of a flow-restricting valve. In some devices, a small valve serves to limit the amount of fluid that can flow out of the eye. The valve is meant to close if the IOP drops too low in order to avoid hypotony, or overly low pressure which can damage the eye. Drainage devices without valves must be temporarily obstructed at the time of implantation in order to avoid hypotony immediately following the procedure, as will be discussed in greater detail below. The type of device used is dependent upon the condition of the eye, particularly the level of IOP and severity of disease, as well as surgeon preference, with numerous factors taken into consideration.
Procedure in Detail
Drainage device surgery is generally performed as an outpatient procedure under local anesthesia with IV sedation- you will be awake but relaxed and will experience no discomfort. After the skin around the eye is cleansed, a surgical drape is placed over the eye to maintain sterility. A small device known as a lid speculum is placed in order to hold open the eyelids during the procedure. The eye is turned downward or upward depending upon where the surgical site will be located, exposing the conjunctiva and sclera. An incision is made in the conjunctiva, which is then carefully lifted and separated from the sclera, and the tissue is carefully dissected in order to create a pocket of space for the device’s plate to be placed. The device is then placed beneath the conjunctiva into the pocket and sutured to the sclera to maintain its position. If the device has no valve, the tube is tied tightly closed with a suture that will dissolve over a six to eight-week period. The tube is then cut to an appropriate length and a small incision is made into the eye, through which the tube is then inserted. The tube is also sutured to the sclera to prevent movement and may then be covered by graft material- usually donor human corneal tissue- which protects it from damage. Once all is in place the conjunctiva is sutured back into its normal position over the plate and tube.
Once surgery is completed, the eye is generally tightly patched and protected by a hard, plastic shield overnight. There is usually minor discomfort and itching. Significant pain is uncommon.
The Day after Surgery
The following morning you will come to the office for a post-operative checkup. The patch and shield will be removed, and the surgeon will check your vision, IOP, and the appearance of the eye, including the plate and tube. At this point instructions regarding acceptable levels of activity and use of postoperative eye drops, including steroids and antibiotics, will be given. It is very important that the drops be taken as prescribed in order that the surgery heals properly. The degree of allowable physical activity, including the ability to drive in the days following surgery, depends on each patient’s unique situation and must be judged individually. In general, strenuous activity, heavy lifting, and bending over should be avoided for the first one to two weeks.
The First Few Weeks after Surgery
Discomfort is generally mild in the first weeks after surgery. The eye may feel a bit sore, and typically there is a scratchy, foreign body sensation due to stitches. Vision is quite variable in these early days, ranging from almost normal to quite blurred. Don’t be alarmed if vision is poor initially, as acuity generally returns to preoperative levels after a few weeks, though may take longer and typically fluctuates quite a bit initially.
You will be monitored closely during the first one to two months following surgery, as this period of time is the most critical to achieving a successful outcome. Corticosteroid eye drops will be taken during this time on a tapering dose schedule and are critical to achieving a good outcome. Antibiotic drops will also be prescribed during the first week. Occasionally, other medications may also be required.
Valved devices will drain immediately, often leading to an initially low IOP that increases over the first few post-operative weeks. Not infrequently, these devices will experience a hypertensive, or high-pressure, phase, often 6-8 weeks after surgery. While additional glaucoma medication may be required to control IOP during this time, they can often be decreased as the pressure drops over the following months.
On the other hand, non-valved devices do not drain at the outset, as they have been tied closed with an absorbable suture. This allows the surrounding tissues time to heal before the suture dissolves and aqueous starts to drain. While non-valved implants may not control IOP as well as valved devices during the first six to eight weeks after surgery, studies show that they lead to lower pressures and somewhat higher success rates in the long term. As noted earlier, the choice of which type of device to implant is made based upon a number of factors taken into account by your surgeon.
Drainage device surgery may lead to a change in the eye’s refractive state, requiring a change in eyeglasses prescription. The eye is usually well healed and stable enough for this at about 8-10 weeks after surgery.
Months to Years after Surgery
Drainage device surgery is generally an effective procedure for IOP reduction, with a 60 to 80% chance of maintaining intraocular pressure at the desired level after one year. Unlike trabeculectomy, in which roughly half of patients need no additional IOP-lowering medication, drainage devices are more likely to require supplemental glaucoma medication to maintain adequate IOP levels. As the years pass it is not unusual for IOP to begin to increase, possibly necessitating the use of additional medications, or additional surgery. In approximately 20 to 40% of cases, surgery fails to adequately control the IOP beyond the first year or two. Additional surgery may then be performed to reach the desired level of pressure within the eye. A second drainage device might be implanted, or other options can be considered.
Patients who have undergone drainage device surgery have an increased lifetime risk of developing an infection inside the eye. Known as endophthalmitis, this kind of infection can seriously harm the eye and lead to loss of vision. The increased risk is due to the opening made in the eye; just as fluid can more easily escape the eye, bacteria can more easily enter. While this risk is generally low, anyone who has undergone drainage device surgery is advised to contact their ophthalmologist immediately if the operated eye ever becomes significantly red or painful, or if vision suddenly decreases. For this reason, the use of contact lenses after drainage device procedures is discouraged.
Risks of Surgery
All surgical procedures carry some risk of complications. Some risks are common to all procedures and patients, and others are more specific to certain types of surgeries or to patients with particular conditions. A thorough explanation of complications will be provided with a surgical consent, should you choose to have surgery, and your physician will review the specific issues you may face based upon your unique circumstances.
Complications
Complications of tube shunts can be divided into early (days to weeks after surgery) or late (months to years after surgery) problems. Some possible surgical complications are noted here:
Early complications:
- Failure to control IOP, as described in detail above
- Bleeding within the eye (hyphema), usually resolves within one week
- Low intraocular pressure (hypotony) resulting in retinal damage (maculopathy), fluid or blood accumulation within the layers of the eye (suprachoroidal fluid or hemorrhage), or shallow anterior chamber
- Wound leak, may require additional sutures
- Double vision, usually resolves after several weeks
- Infection within the eye (endophthalmitis)
- Loss of central vision, rarely severe loss
Late complications:
- Cataract (clouding of the lens of the eye)- development or progression of cataract is fairly common after tube shunt surgery, and may necessitate surgery for cataract removal in subsequent years
- Drooping eyelid (ptosis)
- Conjunctival leak or device exposure, due to breakdown of conjunctiva over the plate or tube, can cause hypotony (see above)
- Infection within the eye (endophthalmitis), risk increases with conjunctival leak or device exposure
- Corneal failure, may require cornea transplant surgery
Alternatives to Glaucoma Drainage Device Surgery
As with most diseases, there are a number of treatment options for glaucoma. As previously noted, surgery is usually considered when medications and laser trabeculoplasty have failed to adequately control IOP. Drainage device surgery, while a commonly performed surgical procedure for glaucoma, is not the only option available. Other surgical procedures may be considered based upon the type of glaucoma, condition of the eye, and level of IOP required. Your surgeon will discuss alternatives for your particular situation, as appropriate. Some of these procedures are detailed in other articles.
Free Lasik Screening
Call 520-355-7501 or Enter Your Information Below!
Please do not submit any Protected Health Information (PHI).
More Categories